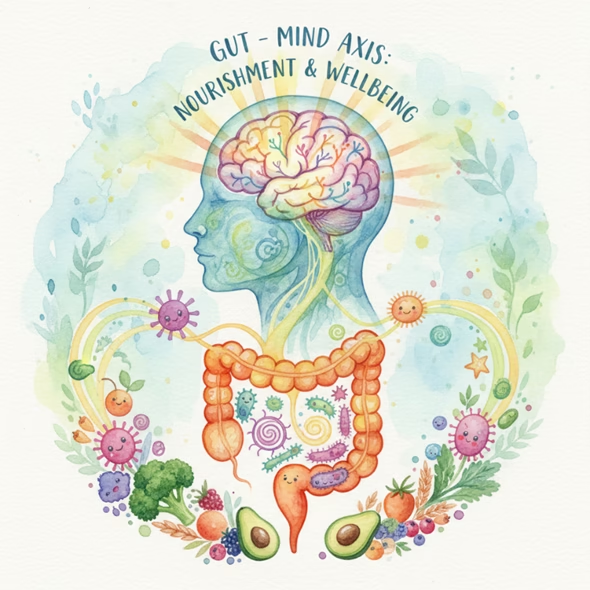
Discover how gut bacteria improves mental disorders and how probiotics, prebiotics, and plant-based foods support mental wellness through the gut-brain connection.
Introduction
Your gut is more powerful than you think — it’s home to over 100 trillion microorganisms forming what scientists call the gut microbiota. Once known only for helping digestion, these bacteria are now recognized as key players in mood, cognition, and emotional health.
Recent research, including a 2023 review published in Nutrients by Sun Yat-sen University, highlights how an imbalance in gut microbes can contribute to conditions like anxiety, depression, bipolar disorder, and autism — and how nutrition and probiotics can help restore harmony.
The Gut-Brain Axis: Your Inner Communication Network
The microbiota–gut–brain axis is a two-way communication system connecting the digestive tract and the central nervous system through neural, hormonal, and immune pathways.
Healthy gut microbes support this dialogue by:
- They produce neurotransmitters like serotonin, dopamine, and GABA that regulate mood and motivation.
- Calming inflammation that can disturb brain chemistry.
- Regulating the HPA axis, which manages stress hormones such as cortisol.
- Generating short-chain fatty acids (SCFAs) like butyrate and propionate that protect neurons and support mental clarity.
When gut balance is lost — a condition called dysbiosis — these pathways break down, leading to higher inflammation, lower serotonin, and altered stress response.
Gut Microbes and Mental Disorders
- Anxiety
People with anxiety often show reduced microbial diversity. They have lower levels of Firmicutes and Faecalibacterium — beneficial bacteria that produce anti-inflammatory SCFAs — and higher levels of Bacteroidetes and Fusobacteria. Restoring gut balance through diet and probiotics can ease anxiety-related symptoms.
- Depression
Studies reveal that depressed patients have higher Prevotella and Clostridium but lower Coprococcus and Dialister. Gut microbes from depressed individuals have even been shown to induce depressive behavior in mice, proving the causal link. Dysbiosis may reduce tryptophan and serotonin levels while raising inflammation.
- Bipolar Disorder
Bipolar patients tend to have fewer Faecalibacterium and more Clostridiaceae and Actinobacteria. Because bipolar episodes involve oxidative stress and inflammation, restoring microbial diversity may help regulate mood stability.
- Autism Spectrum Disorder (ASD)
Children with ASD often have more Clostridium and fewer Faecalibacterium and Akkermansia muciniphila. These imbalances can influence serotonin metabolism, worsening sensory and sleep issues. Nutritional modulation and probiotics are being explored as supportive therapies.
- Schizophrenia and Others
Patients with schizophrenia show fewer Ruminococcus and Roseburia (butyrate producers) and more Lactobacillus fermentum and Enterococcus faecium. Such microbial shifts may alter neurotransmitters like glutamate and GABA, affecting cognition and perception.
The message is clear — mental health begins in the gut.
Feeding the Mind : Nutrition That Nourishes Your Microbes
- Probiotics: Friendly Bacteria for a Balanced Mind
Probiotics such as Lactobacillus and Bifidobacterium restore microbial equilibrium and calm stress responses.
L. rhamnosus and L. reuteri raise GABA in the brain and reduce anxiety in animal models.
L. rhamnosus HN001 lowered postpartum anxiety in human trials.
Multi-strain probiotic blends improved mood, sleep, and cognition better than single strains.
Probiotics work by modulating the HPA axis, increasing serotonin, and boosting brain-derived neurotrophic factor (BDNF).
- Prebiotics and Postbiotics: Feeding the Good Guys
Prebiotics such as galacto-oligosaccharides (GOS) and inulin feed beneficial bacteria. GOS intake has been linked to reduced anxiety and better emotional regulation.
Meanwhile, short-chain fatty acids (SCFAs) — the postbiotics produced by bacterial fermentation — protect the brain and strengthen the gut barrier.
When combined, synbiotics (probiotics + prebiotics) can enhance both gut and psychological well-being.
- Fermented Dairy and Plant Foods
Fermented foods like yogurt, kefir, and kimchi are natural sources of probiotics.
Clinical studies show that fermented dairy drinks containing Lactobacillus paracasei or L. plantarum increased beneficial microbes and reduced depressive symptoms.
However, choose low-sugar or naturally fermented products, as added sugars can offset gut benefits.
- Spices and Botanicals with Psychobiotic Power
Nature’s pantry holds remarkable microbiome boosters:
Curcumin (turmeric) reduces inflammation and rebalances gut flora.
Capsaicin (chili pepper) improves gut composition and decreases depressive behavior.
Zanthoxylum bungeanum, a traditional Asian spice, helps relieve stress and oxidative damage.
- Fruits, Vegetables, and Herbs for Mental Wellness
Plant-based diets rich in fibre and polyphenols consistently correlate with lower depression rates.
Flavonoid-rich orange juice and antioxidant-dense herbs like Ginseng, Ginkgo biloba, and Goji berry increase beneficial bacteria and BDNF levels — the brain’s “growth fertilizer.”
These findings reinforce that what you eat daily can either nourish or neglect your emotional health.
Personalized Nutrition: The Future of Gut-Based Therapy
Every microbiome is unique — almost like a genetic signature. The next stage of mental-gut medicine is personalization.
By identifying individual microbial profiles, practitioners can tailor probiotic strains, dietary plans, or even postbiotic formulations to each person’s needs.
However, more human-level studies are needed to pinpoint the right species and doses for specific disorders. Until then, a whole-food, fibre-rich diet remains the safest way to keep your microbes thriving.
5 Everyday Ways to Support Gut-Driven Mental Wellness
- Feed your microbes with colorful, fiber-rich foods.
- Add fermented foods — yogurt, kefir, kimchi, sauerkraut — to your diet.
- Spice smartly with turmeric, chili, and pepper for their anti-inflammatory benefits.
- Limit processed foods and sugar, which disrupt gut balance.
- Consider a clinically tested probiotic under healthcare guidance for extra support.
Conclusion: Healing the Mind from the Inside Out
The gut microbiota isn’t just a digestive assistant — it’s an emotional regulator, immune coach, and brain ally.
Imbalances in these microscopic communities can lead to emotional distress, but nourishing them through diet, probiotics, and lifestyle can restore harmony.
At Nutrify Your Gut, we believe wellness starts within. A nourished gut leads to a calmer mind, sharper focus, and deeper resilience.
✨ Feed your microbes — and let them feed your happiness. ✨
Reference : https://pmc.ncbi.nlm.nih.gov/articles/PMC10384867/pdf/nutrients-15-03258.pdf


