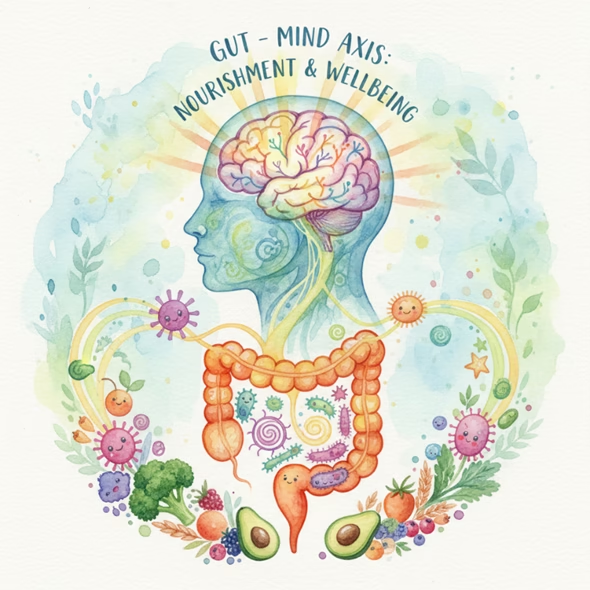
Discover why the gut is called the body’s “second brain” and how your microbiota, diet, and lifestyle influences emotions, immunity, and long-term health.
Introduction: Your Gut Thinks, Feels, and Talks to Your Brain
The phrase “gut feeling” is more than just intuition — it’s science. Inside your digestive tract lives a vast network of over 100 million neurons, known as the enteric nervous system (ENS). This “second brain” operates independently yet communicates constantly with your central nervous system through the vagus nerve.
At the same time, trillions of microorganisms — your gut microbiota — form a thriving ecosystem that influences not just digestion, but also mood, sleep, immunity, and even decision-making.
Recent studies show that gut microbes affect the brain via neural, hormonal, and immune pathways, shaping mental health and cognitive function. Understanding this connection unlocks new possibilities for managing anxiety, depression, neurodegenerative disorders, and overall well-being.
The Science Behind the Gut–Brain Axis
The gut and brain are in constant communication — a bi-directional feedback loop scientists call the microbiota–gut–brain axis.
The vagus nerve carries information from the gut to the brain, regulating digestion, appetite, and emotional responses.
Gut microbes produce neurotransmitters such as serotonin, dopamine, and GABA, which directly influence mood and cognition.
Short-chain fatty acids (SCFAs) like butyrate, acetate, and propionate are produced when microbes digest dietary fibre, and they nourish intestinal cells, reduce inflammation, and support neural signalling.
The immune system acts as a mediator: when the gut is inflamed or imbalanced, immune messengers (cytokines) can affect brain chemistry, increasing the risk of mental distress.
Simply put: when your gut thrives, your brain flourishes.
Gut Microbes and the Enteric Nervous System: A Powerful Duo
The enteric nervous system (ENS) — sometimes called the “little brain in your gut” — contains more neurons than your spinal cord. It controls the rhythmic contractions that move food through your digestive tract and manages the release of digestive enzymes and hormones.
But the ENS doesn’t work alone. It collaborates closely with your gut microbiota and immune system to maintain a stable intestinal environment. Together, these systems form the foundation of both physical and mental resilience.
When the microbial balance shifts — a state called dysbiosis — the ENS can become overstimulated or underactive, leading to conditions like irritable bowel syndrome (IBS), depression, or anxiety.
How Lifestyle and Diet Influence Your Second Brain
- Diet: The Primary Shaper of Gut Microbiota
While genetics influence which microbes can colonize your gut, diet is the strongest modulator of microbial diversity and health. Research shows:
Diets rich in plant-based foods, fiber, and polyphenols (found in fruits, vegetables, and whole grains) promote beneficial bacteria that produce SCFAs — key for brain and gut function.
Fermentable fibers (prebiotics) act as food for healthy microbes, improving intestinal balance.
Omega-3 fatty acids (found in fish, walnuts, and flaxseeds) enhance the intestinal barrier and support brain signaling.
Conversely, Western-style diets high in sugar, processed fats, and refined carbohydrates reduce microbial diversity and fuel inflammation — a risk factor for both gut and mood disorders.
A diet that feeds your microbes truly feeds your mind.
- Probiotics and Fermented Foods: The Good Bacteria Boost
Consuming probiotic-rich foods like yogurt, kefir, kombucha, and fermented vegetables helps replenish beneficial bacteria such as Lactobacillus and Bifidobacterium.
Clinical studies reveal that probiotic supplementation can:
- Reduce symptoms of anxiety and depression
- Lower cortisol (the stress hormone)
- Enhance serotonin and dopamine pathways
- Improve sleep quality and cognitive function
For long-term benefits, combine probiotics with prebiotics — fibers found in garlic, onions, bananas, and oats — to nourish these friendly microbes.
- Exercise and Environment: Non-Dietary Gut Boosters
Physical activity doesn’t just tone muscles — it strengthens the gut-brain link. Regular moderate exercise increases microbial diversity and boosts SCFA production.
Likewise, reducing smoking and alcohol consumption preserves beneficial bacteria and lowers inflammation.
Even spending time outdoors can help — environmental exposure introduces diverse microbes that enhance immune balance and gut resilience.
The Gut and Mental Health: The Emotional Connection
The gut microbiota influences the brain through chemical signaling. About 90% of serotonin, the neurotransmitter that regulates happiness and mood, is produced in the gut.
When microbial diversity decreases, serotonin production drops, and inflammation rises — a combination strongly linked to depression and anxiety.
Several mental health conditions have been associated with gut imbalance:
- Depression: Reduced beneficial bacteria such as Faecalibacterium and Coprococcus, and elevated inflammatory microbes.
- Anxiety: Altered Firmicutes/Bacteroidetes ratio and low GABA-producing species.
- Alzheimer’s & Parkinson’s: Disrupted gut microbiota linked to neuroinflammation and cognitive decline.
Encouragingly, restoring gut balance through nutrition, lifestyle, and probiotic therapy has shown promise in reducing symptoms across these disorders.
Practical Steps to Nurture Your Gut–Brain Connection
- Eat more whole, plant-based foods — at least five servings of fruits and vegetables daily.
- Include prebiotic fibers (like oats, garlic, leeks, and legumes) to feed good bacteria.
- Add fermented foods such as yogurt, kefir, kimchi, or sauerkraut for live probiotics.
- Choose healthy fats — omega-3-rich foods like salmon, flaxseeds, or walnuts support gut lining integrity.
- Limit processed foods and refined sugars that promote inflammation.
- Move daily — even 30 minutes of brisk walking can enhance microbial balance.
- Stay hydrated and manage stress through mindfulness or yoga to protect your gut-brain axis.
- Avoid unnecessary antibiotics and smoking — both harm microbial diversity.
These small, consistent habits build a stronger gut ecosystem, which in turn fosters emotional balance and mental clarity.
The Future of Gut-Based Therapy
As research advances, the gut microbiome is emerging as a therapeutic target for mental health. Scientists are exploring psychobiotics — probiotic strains specifically designed to influence mood and cognition — as natural adjuncts to conventional treatments.
Additionally, precision nutrition and microbiome mapping could soon allow personalized diets that optimize both gut and brain function.
While more studies are needed, one thing is clear: healing begins in the gut.
Conclusion: Listen to Your Second Brain
Your gut isn’t just a digestive organ — it’s a neurological powerhouse that shapes how you think, feel, and function.
By eating mindfully, moving regularly, and supporting your microbiota with natural foods and probiotics, you nurture not just your gut — but your whole self.
At Nutrify Your Gut, we believe that every meal is an opportunity to feed your second brain and enhance your mental and physical well-being.
✨ Trust your gut — it truly knows what your brain needs. ✨
References :
Suggested Tags: Gut Health, Microbiome, Mental Health, Gut-Brain Axis, Probiotics, Holistic Nutrition, Psychobiotics
Slug / URL: /blog/gut-brain-connection-second-brain
Focus Keywords:
- gut-brain connection
- gut microbiota and mental health
- second brain
- probiotics and mood
- gut health diet
- enteric nervous system